A team of researchers from Harvard Medical School and Boston Children’s Hospital has developed a device to help patients experiencing refractory hypoxemia. In their paper published in Proceedings of the National Academy of Sciences, the group describes their new device and how well it worked when tested on human blood and blood inside of live rats.
Refractory hypoxemia is a condition sometimes experienced by patients on ventilators—it is generally due to acute respiratory distress syndrome. Less oxygen makes the trip from the lungs into the bloodstream, leading to organ damage and sometimes death. Current treatment often involves the use of an extracorporeal membrane oxygenation (ECMO) machine. It extracts most of a patient’s blood, removes carbon dioxide, adds oxygen and then pumps it back into the patient. Because ventilators can damage lungs, and because access to ECMO machines is limited (and risk of infection is high), the researchers developed a new machine that can add oxygen directly to blood while it is still inside the patient.
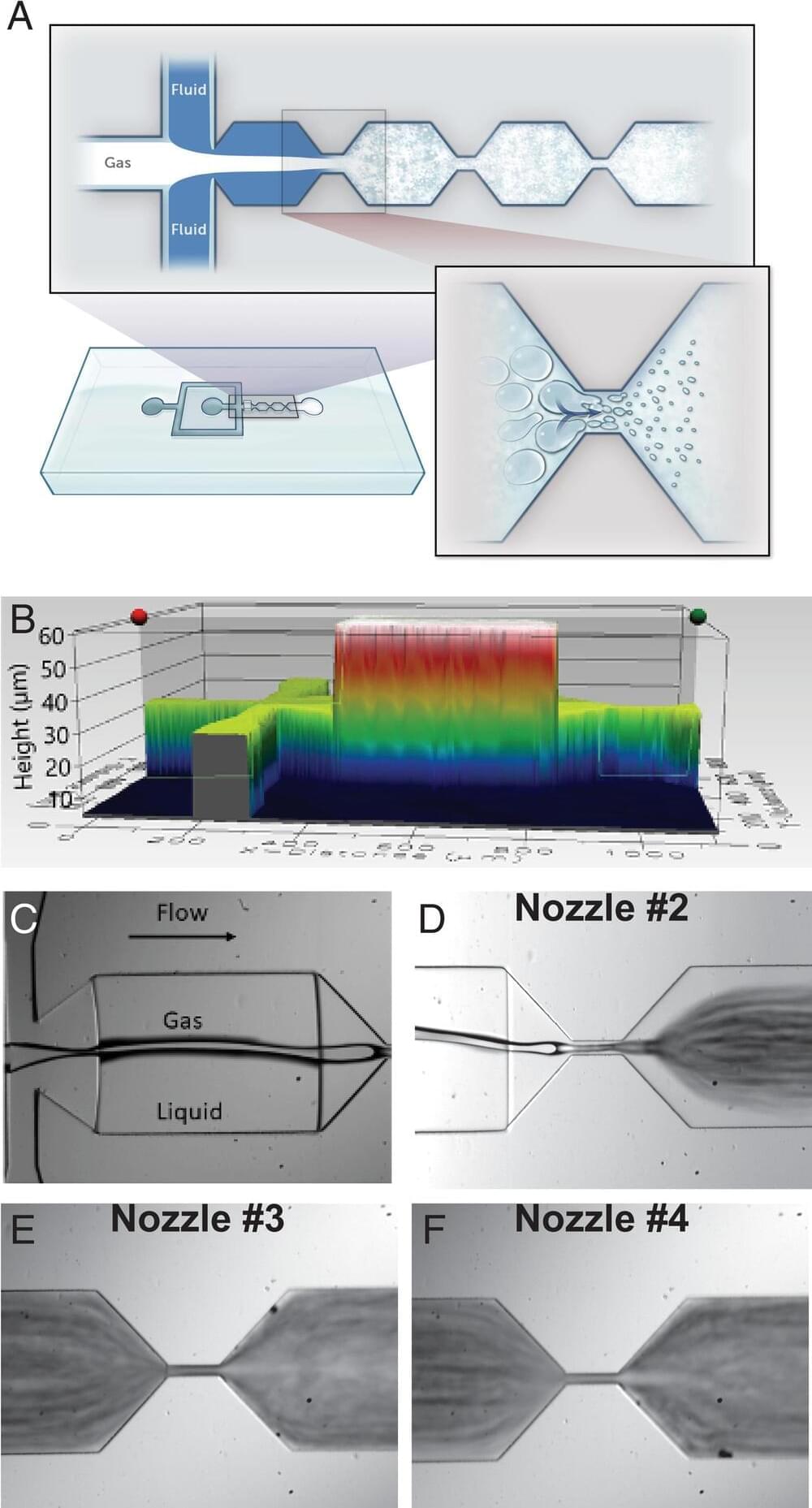
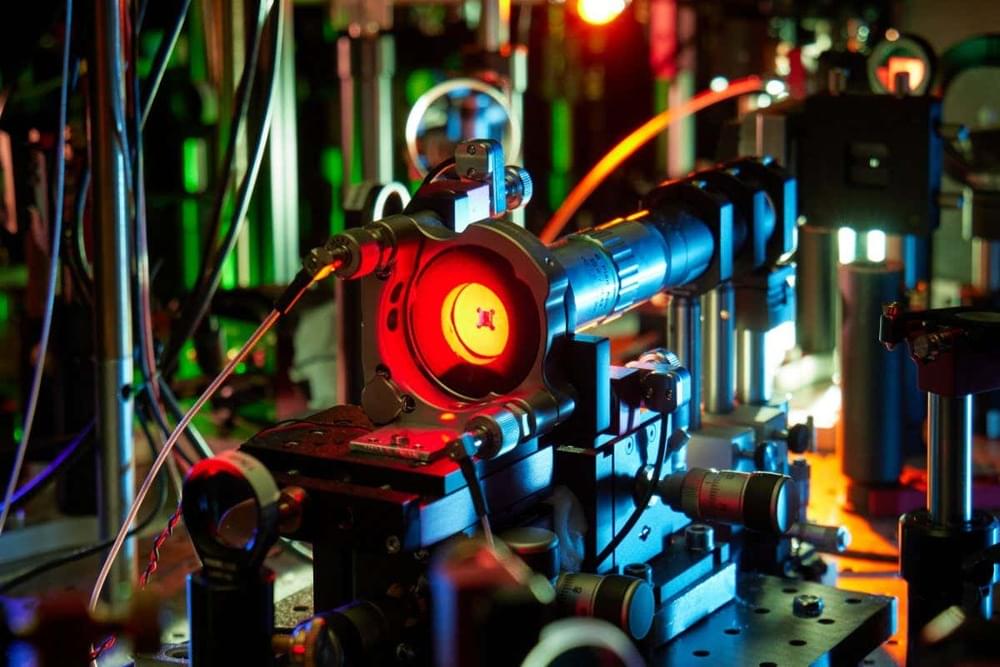
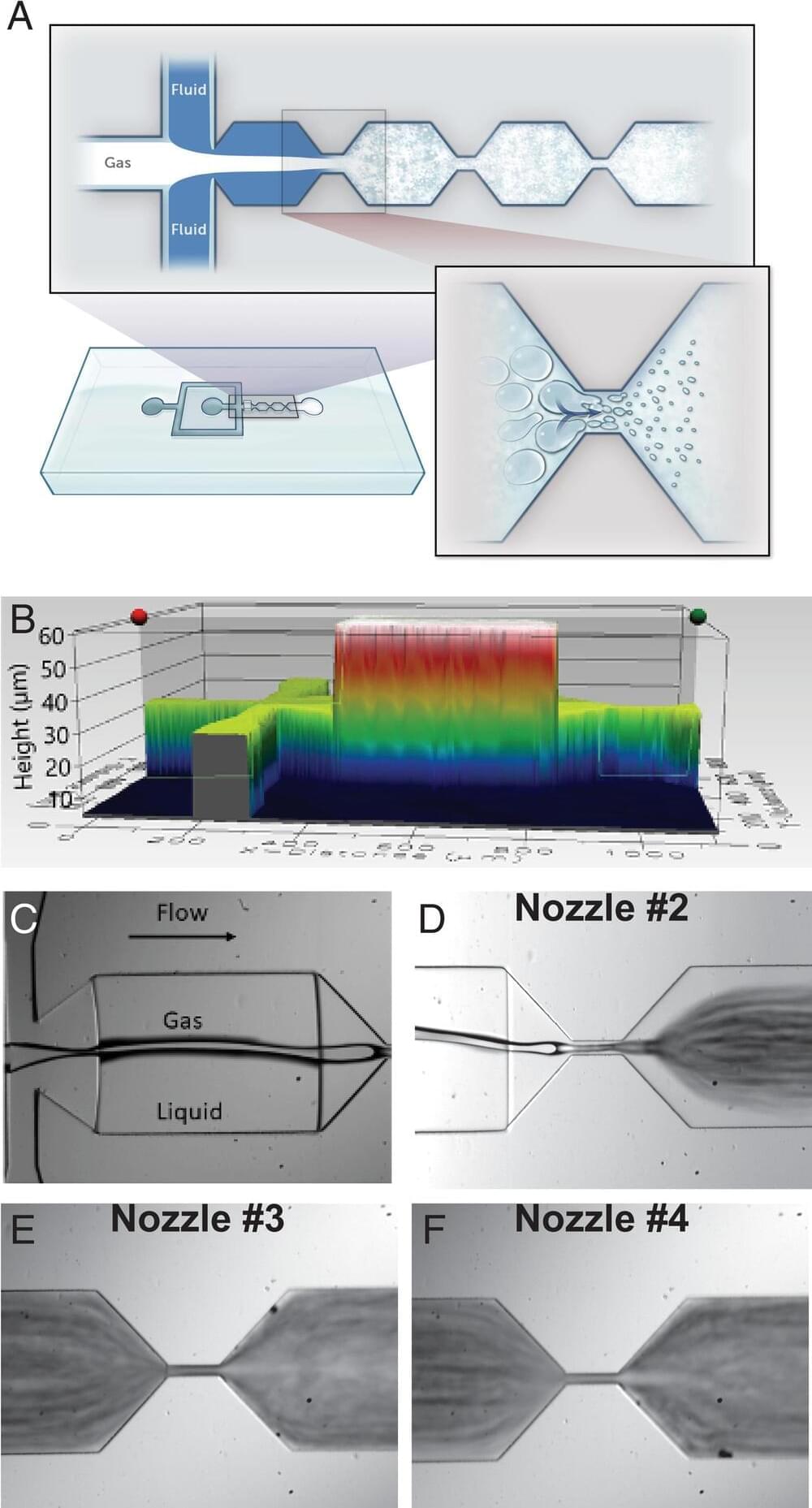
The new machine works by first infusing oxygen into a liquid solution. That solution travels through a series of ever-smaller nozzles, reducing the size of the bubbles down to micron scale. The bubbles, the researchers note, are smaller than red blood cells. Next, the bubbles get a coating of a lipid membrane that is similar to some types of natural cell membranes. This prevents toxicity and also keeps the bubbles from sticking together. The resulting solution is then injected directly into a patient’s bloodstream. Once inside, the lipids dissolve, releasing the oxygen into the bloodstream. They are tiny enough that they will not block any blood vessels.