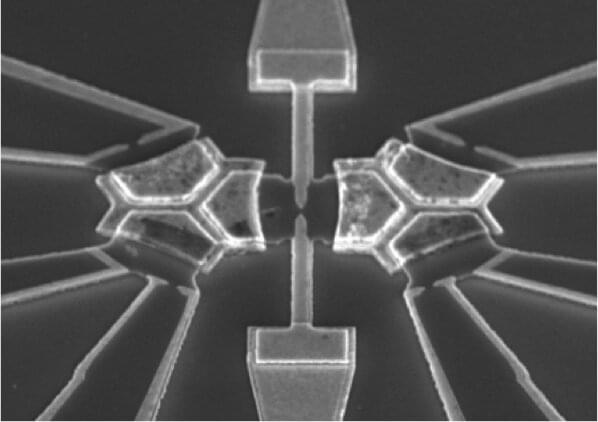
Radiotherapy (RT) is an established treatment modality of malignant tumors. Currently, photon beam therapy is the most widely used in clinical settings. Intensity-modulated photon radiotherapy (IMRT) was introduced in the mid-1990s, and it took the radiotherapy with photons to a huge leap forward. As the development of IMRT, it has been considered to be the advanced and the standard of treatment for many malignancies [1]. Although the IMRT technique can typically provide a more conformal dose distribution than the traditional RT mode, it is necessary to improve the tumor control and overall survival (OS), and reduce the RT toxicity. It is well known that the advantage of a proton beam is the physical characteristics of its depth-dose curve, with a dose peak (Bragg peak) at a well-defined depth in tissue (Fig. 1). For relatively shallow tumors, unlike the photon depth-dose curve showing an exponentially decreasing energy deposition with increasing depth in tissue, the Bragg peak allows for rapid fall-off of the radiation dose at the end of the range and a sharp lateral dose fall-off with the maximum energy deposition for each proton beam in the target region and almost no energy around it. Therefore, proton beam therapy (PBT) effectively allows the delivery of high-radiation doses to tumor cells and very low or zero doses to the normal cells, which is recognized as an ideal therapy modality for treatment of malignant diseases, especially for organs at risk (OARs) with less toxicity. As Dr. Herman Suit in the department of radiation oncology of Massachusetts General Hospital (MGH) said: “No advantage to any patient for any irradiation of any normal tissue exists; and radiation complication never occurs in nonirradiated tissues.”
In 1946, Robert R. Wilson proposed to use accelerator-produced beams of protons to treat patients with deep-seated tumors [2]. In 1954, the first patient with breast cancer was treated with proton radiation of the pituitary in the Berkeley Radiation Laboratory [3]. In 1961, protons commenced to be used for clinical treatment at Harvard Cyclotron Laboratory [4]. Initially, the clinical practice and research of PBT only focused on the tumors near a critical structure or those that responded poorly to photon radiotherapy such as ocular tumors, skull base tumors, paraspinal tumors, and unresectable sarcomas. Over the next 60 years, with the vast development of technology, the application of PBT has been gradually expanding to various neoplasms. Although increasingly more evidence has been indicated for the advantages of PBT in clinical experience, PBT is not good for all cases all of the time. It is very important to understand the benefits and limitations of protons as well as the biology and the behavior of the tumor. In this review, we summarized the latest advances and clinical applications of PBT. We also considered the challenges of treatment optimization in the era of precision medicine.