The ruling is a tougher version of China’s ban of wildlife meat, after it was linked to the virus.


In the stillness and noise of the M.R.I., I picture what the magnet is doing to my brain. I imagine hydrogen protons aligning along and against the direction of its field. Bursts of radio waves challenge their orientation, generating signals that are rendered into images. Other than the sting of the contrast agent, the momentary changes in nuclear spin feel like nothing. “Twenty-five more minutes,” the radiologist says through the plastic headphones. Usually, I fall asleep.
I’ve had more than 50 scans since 2005, when I received a diagnosis of multiple sclerosis, and I now possess thousands of images of my brain and spine. Sometimes I open the files to count the spinal-cord lesions that are slowly but aggressively taking away my ability to walk. On days my right leg can clear the ground, it feels as if a corkscrew is twisting into my femur. I take halting steps, like a hapless robot, until it’s impossible to move forward. “Maybe in 10 years there will be a pill, or a treatment,” a doctor told me.
For now, even a sustained low fever could cause permanent disability, and medications that treat the disease have left me immunosuppressed, making fevers more likely. I quarantined before it was indicated, and what I miss most now, sheltering in place, are walks through my neighborhood park in Los Angeles with my dog, who gleefully chases the latest bouncy ball I’m hurtling against the concrete. Her current favorite is the Waboba Moon Ball, which comes in highlighter fluorescent yellow and Smurf blue, among other colors. Technically Moon Balls are spherical polyhedrons. They sport radically dimpled surfaces, as if Buckminster Fuller had storyboarded an early pitch for “Space Jam.” Moon Balls are goofy, but they bounce 100 feet.
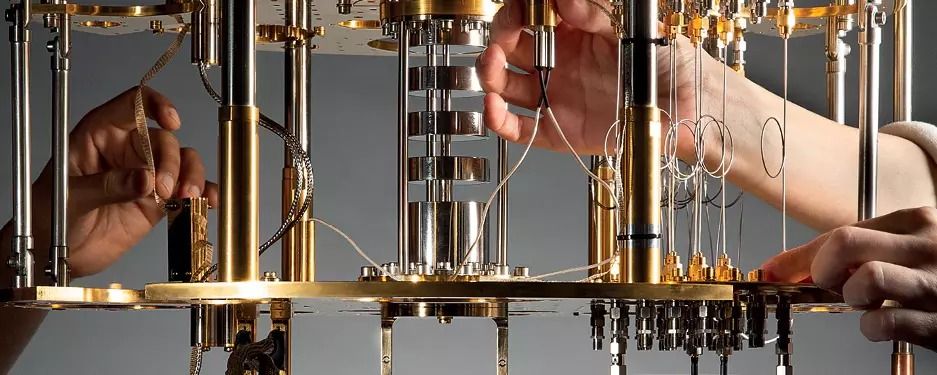
It’s been said that quantum computing will be like going from candlelight to electric light in the way it will transform how we live. Quite a picture, but what exactly is quantum computing?
For the answer to that question, we’ll have to visit a scale of existence so small that the usual rules of physics are warped, stretched and broken, and there are few layperson terms to lean on. Strap yourself in.
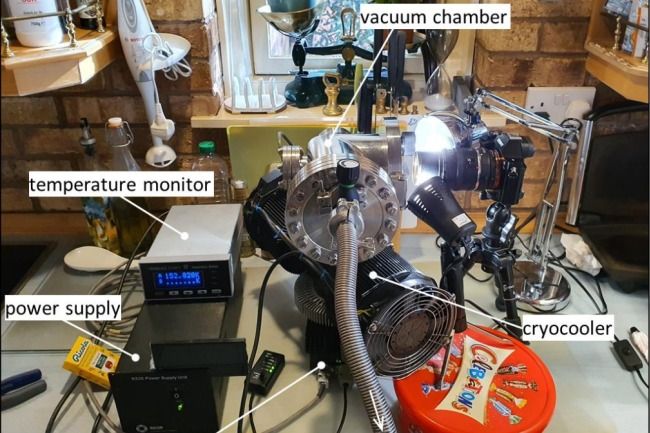
Luckily, we have a world-leading researcher in quantum computing, Professor David Reilly, to guide us. “Most modern technologies are largely based on electromagnetism and Newtonian mechanics,” says Reilly in a meeting room at the University’s Nano Hub. “Quantum computing taps into an enormous new area of nano physics that we haven’t harnessed yet.”
Some foresee quantum computers will come to solve some of the world’s most serious issues. However, others accept that the advantages will be exceeded by the downsides, for example, cost or that quantum computers basically can’t work, incapable to play out the complexities demanded of them in the manner we envision. The integral factor will be if the producers can guarantee ‘quantum supremacy’ by accomplishing low error rates for their machines and outperforming current computers.
Hollywood has made numerous anticipations with respect to the future and artificial intelligence, some disturbing, others empowering. One of the most quickly developing research areas takes a look at the use of quantum computers in molding artificial intelligence. Actually, some consider machine learning the yardstick by which the field is estimated.
The idea of machine learning, to ‘learn’ new data without express explicit instruction or programming has existed since 1959, in spite of the fact that we still haven’t exactly shown up at the vision set somewhere by the likes of Isaac Asimov and Arthur C. Clarke. In any case, the conviction is that quantum computing will help accelerate our advancement right now. What was at one time a periphery thought evaded by the more extensive science community, has developed to turn into a well known and practical field worthy of serious investment.


This week, the U.S. government approved the first blood test in the country that will look for the antibodies produced by the body to fight the novel coronavirus. Such a test can reveal whether someone is actively infected by the virus, as well as whether they were previously infected but recovered. While these tests are very much needed to better understand the scale of the outbreak, they have a few major limitations.
On Thursday, the Food and Drug Administration issued an Emergency Use Authorization to a covid-19 antibody test developed by the company Cellex. The test looks for two types of antibodies, IgM and IgG, created by the body’s immune system in response to the new coronavirus, known as SARS-CoV-2. The test, which requires blood drawn from a vein, can return results within 15 to 20 minutes, though the testing itself has to be done in a certified laboratory, not at a doctor’s office, unlike some other rapid covid-19 tests.


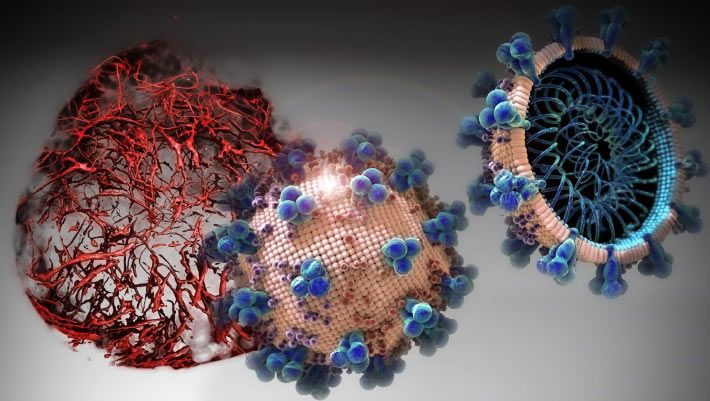
A trial drug called APN01 or human recombinant soluble ACE2 (hrsACE2) can significantly block early stages of SARS-CoV-2 infections, according to a paper published in the journal Cell.