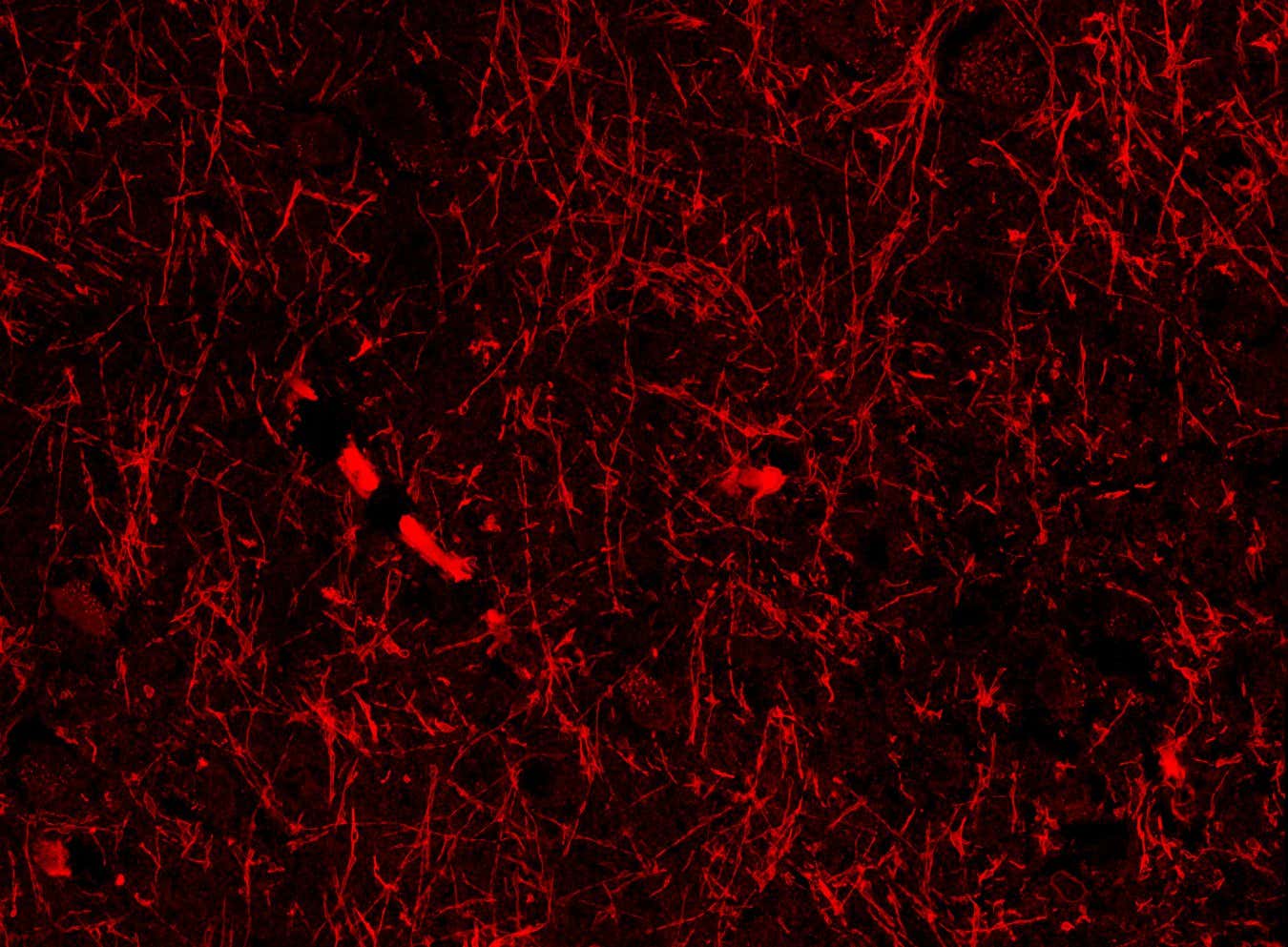
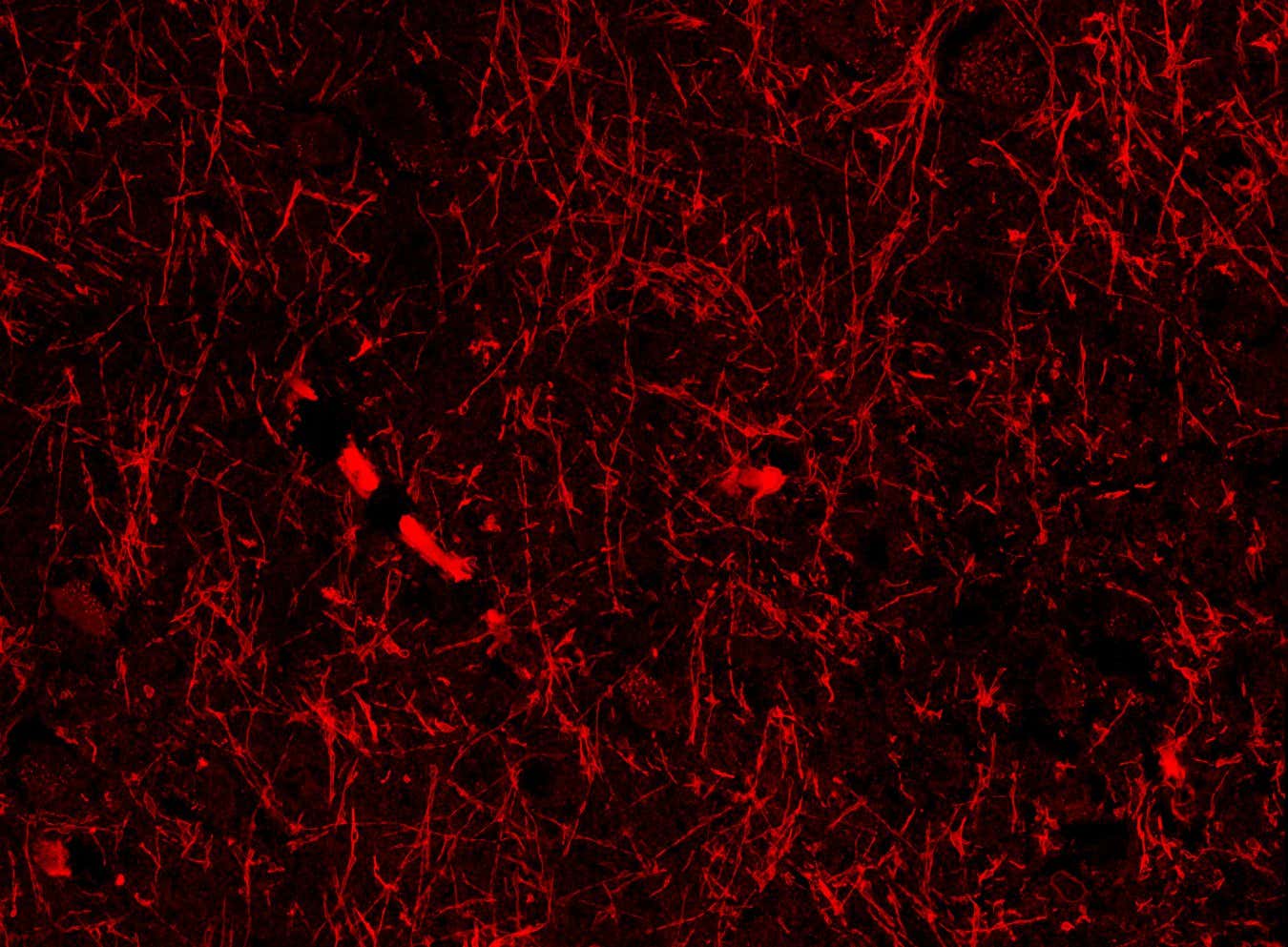
Scientists may have stumbled across a network of vessels in the brain that helps clear out waste fluid – a discovery that could “represent a paradigm shift in our understanding of all neurodegenerative diseases”

What if worn-out parts of your body didn’t need to be replaced just regenerated?
Stanford researchers recently published work showing cartilage lost to aging or arthritis can be regrown, using either an oral drug or a local injection.
If this translates to humans, it could make knee and hip replacements unnecessary.
Millions of people undergo major joint replacement surgery every year.
Regenerating cartilage instead of replacing joints would mean less pain, lower cost, and far better outcomes.
That future may be closer than we think.
Complex eyes in vertebrates may have evolved as early as 500 million years ago. Reconstructing the early evolutionary history of vertebrates requires understanding organisms that existed before bone evolved. However, these ‘soft-bodied’ fossils are inherently difficult to study, resulting in conflicting anatomical and evolutionary interpretations. For the first time, researchers used synchrotron-based imaging techniques to examine two Silurian taxa, Jamoytius and Lasanius, that may bridge the gap between the bone-less and boned vertebrates. They recover the first direct evidence of biomineralised apatitic bone in both taxa and of camera-eyes in Jamoytius. The discoveries indicate vertebrate bones and complex eyes evolved earlier than previously thought, and demonstrate the power of these techniques for problematic fossils.
Read the article in Proceedings B.
Abstract. Understanding the origin and early diversification of vertebrates has always been a challenge because of the ambiguous and conflicting interpretations of the soft-bodied, pre-biomineralization fossil record. Here, we apply synchrotron radiation techniques to Jamoytius and Lasanius, two soft-bodied Silurian vertebrates, key taxa for discerning vertebrate bone evolution owing to highly localized, but debated, biomineralization. We map soft-tissue structures and quantify details of biochemical residue impossible to resolve with traditional methods. We present the first unequivocal evidence for biomineralized apatitic scales in Jamoytius by combining synchrotron rapid scanning X-ray fluorescence and Fourier transform infrared spectroscopy (elevated Ca 37% and P 21%). This approach also recovers robust evidence for apatitic biomineralization in Lasanius. Chemical mapping of the optical anatomy of Jamoytius recovers a close correlation with Zn and Cu distribution, providing evidence for a retinal pigmented epithelium and complex eyes. In both taxa, chemical maps reveal original anatomical details not apparent in visible light, including potential evidence of other sensory anatomy in Jamoytius. Our work resolves long-standing fundamental anatomical debates, indicating stem-group origins for bone and complex eyes in vertebrates. We highlight the potential of using a powerful combination of analytical techniques to unlock otherwise inaccessible data in problematic fossils.
🌏 Get Exclusive NordVPN 2Y deal + 4 months extra here → https://nordvpn.com/sabine It’s risk-free with Nord’s 30-day money-back guarantee! ✌️
In the many worlds theory of quantum physics, all possible outcomes of a quantum event occur, creating branching parallel worlds in which a different outcome is reality. According to a recently published paper, communication between those worlds should be possible under our current understanding of quantum physics. Sounds crazy? Let’s take a look.
Paper: https://arxiv.org/abs/2601.
👕T-shirts, mugs, posters and more: ➜ https://sabines-store.dashery.com/
💌 Support me on Donorbox ➜ https://donorbox.org/swtg.
👉 Transcript with links to references on Patreon ➜ / sabine.
📝 Transcripts and written news on Substack ➜ https://sciencewtg.substack.com/
📩 Free weekly science newsletter ➜ https://sabinehossenfelder.com/newsle… Audio only podcast ➜ https://open.spotify.com/show/0MkNfXl… 🔗 Join this channel to get access to perks ➜ / @sabinehossenfelder 📚 Buy my book ➜ https://amzn.to/3HSAWJW #science #sciencenews #physics #quantum.
👂 Audio only podcast ➜ https://open.spotify.com/show/0MkNfXl…
🔗 Join this channel to get access to perks ➜
/ @sabinehossenfelder.
📚 Buy my book ➜ https://amzn.to/3HSAWJW
#science #sciencenews #physics #quantum
We usually think of the past as something that no longer exists. It happened — and then it disappeared. But modern physics challenges this intuition in a profound way.
In this video, we explore why the past may still exist — not as memory, but as structure.
Drawing on ideas associated with Leonard Susskind, this documentary examines how relativity and modern spacetime physics reshape our understanding of time. In Einstein’s framework, there is no universal “now.” What is past for one observer may be present or future for another, depending on motion and frame of reference.
This destroys the idea that the past vanishes.
In the spacetime view, the universe is a four-dimensional structure. Events are not erased — they are located. The past is not something that disappeared. It is something that exists in a different region of spacetime.
From this perspective, time does not flow in the way we imagine. The sense of disappearance comes from human experience, not from fundamental physics.
SpaceX, in collaboration with xAI, plans to build a lunar base called Moonbase Alpha using advanced technologies such as mass drivers, solar power, and Starship, aiming to make human activity on the moon visible, affordable, and sustainable ##
## Questions to inspire discussion.
Launch Infrastructure Economics.
🚀 Q: What launch costs could SpaceX’s moon infrastructure achieve? A: Mature SpaceX moon operations could reduce costs to $10/kg to orbit and $50/kg to moon surface, enabling $5,000 moon trips for people under 100kg (comparable to expensive cruise pricing), as mentioned by Elon Musk.
⚡ Q: How could lunar mass drivers scale satellite deployment? A: Lunar mass drivers using magnetic rails at 5,600 mph could launch 10 billion tons of satellites annually with 2 terawatts of power, based on 2023 San Jose State study updating 1960s-70s mass driver literature.
Starship Capabilities.
Optimus robots, with their rapidly advancing capabilities in AI and dexterity, are poised to revolutionize the field of surgery, potentially surpassing human surgeons in precision and accessibility within a few years and making traditional surgical expertise and even medical school obsolete.
## Questions to inspire discussion.
Healthcare Access & Economics.
🏥 Q: How will Optimus robots change healthcare costs and accessibility?
A: Optimus surgeon robots will operate at costs limited to capital expenditure and electricity, enabling deployment in rural villages and developing countries like Zimbabwe and throughout Africa, demonetizing and decentralizing access to medical care that will exceed what presidents currently receive.
Technology Timeline & Capabilities.
Claude Opus 4.6 and GPT 5.3 Codex, two AI models, have different strengths and interaction styles, highlighting the trade-offs between elegance, reliability, and efficiency in their performance ##
## Questions to inspire discussion.
Model Selection Strategy.
🎯 Q: Which AI model should I choose for different programming tasks?
A: Use Opus for interactive roleplay and quick command following with trial-and-error workflows, while Codex excels at delivering elegant solutions when given proper context and reads more code by default.
🔄 Q: How long does it take to effectively switch between AI models?