Neuralink achieved two brain transplants in a day, targeting 20 by year-end. CEO Elon Musk envisions healing paralysis and blindness.
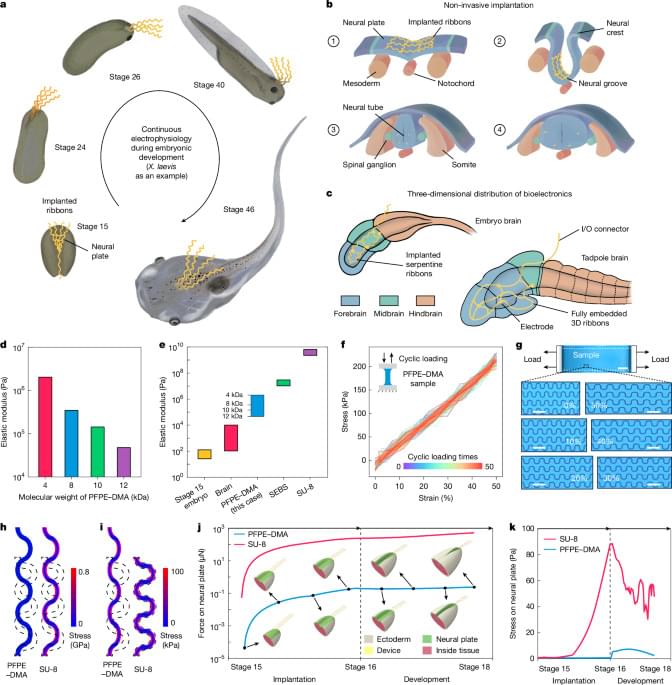
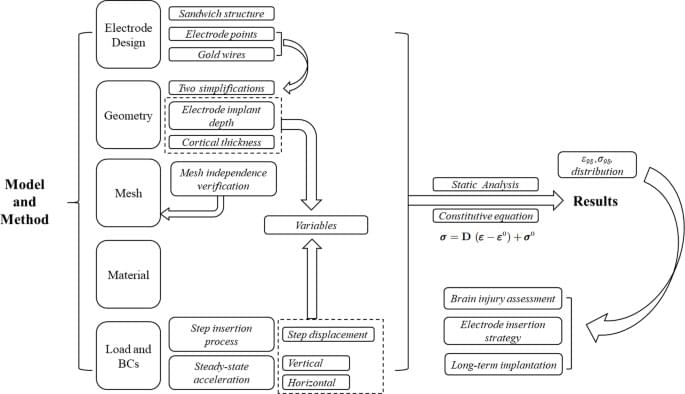
Peng, L., Wang, L., Wu, S. et al. Sci Rep 15, 19,938 (2025). https://doi.org/10.1038/s41598-025-04737-3
It’s 3:43 AM. Sirens are howling. Your phone lights up: DEFCON 1. Multiple ICBMs inbound.
World War 3 has just begun.
Would you know what to do in the first minutes? Most people freeze. This guide is for those who act.
In this video, we walk you through the real first steps to take if global war breaks out — not theory, not panic, but practical survival strategy for the first 24 hours: from identifying if you’re in a high-risk zone, to securing water and food, to communicating with loved ones when the grid is down.
💥 Whether it’s a nuclear attack, an EMP, or a cyber blitz — this is what you need to know before it’s too late.
Topics we cover include:
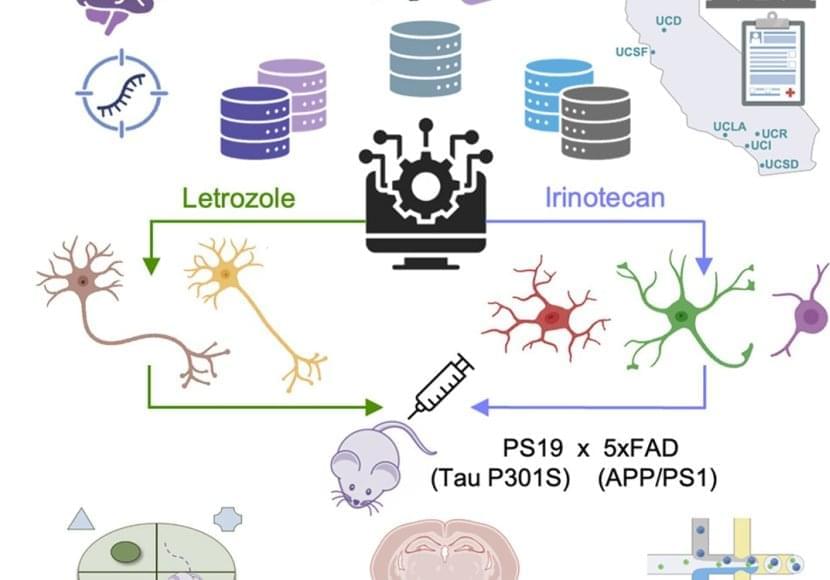
The team took publicly available data from three studies of the Alzheimer’s brain that measured single-cell gene expression in brain cells from deceased donors with or without Alzheimer’s disease. They used this data to produce gene expression signatures for Alzheimer’s disease in neurons and glia.
The researchers compared these signatures with those found in the Connectivity Map, a database of results from testing the effects of thousands of drugs on gene expression in human cells.
Out of 1,300 drugs, 86 reversed the Alzheimer’s disease gene expression signature in one cell type, and 25 reversed the signature in several cell types in the brain. But just 10 had already been approved by the FDA for use in humans.
Poring through records housed in the UC Health Data Warehouse, which includes anonymized health information on 1.4 million people over the age of 65, the group found that several of these drugs seemed to have reduced the risk of developing Alzheimer’s disease over time.
“Thanks to all these existing data sources, we went from 1,300 drugs, to 86, to 10, to just 5,” said the lead author of the paper.
The authors chose 2 cancer drugs out of the top 5 drug candidates for laboratory testing. They predicted one drug, letrozole, would remedy Alzheimer’s in neurons; and another, irinotecan, would help glia. Letrozole is usually used to treat breast cancer; irinotecan is usually used to treat colon and lung cancer.
The team used a mouse model of aggressive Alzheimer’s disease with multiple disease-related mutations. As the mice aged, symptoms resembling Alzheimer’s emerged, and they were treated with one or both drugs.
Enhancing Functional Independence For Older Adults — Dr. On-Yee “Amy” Lo, Ph.D. — Marcus Institute for Aging Research / Harvard Medical School.
Dr. On-Yee (Amy) Lo, Ph.D. is Assistant Scientist II at the Marcus Institute for Aging Research (https://www.marcusinstituteforaging.org/who-we-are/profiles… and Assistant Professor of Medicine, Harvard Medical School and Beth Israel Deaconess Medical Center (https://connects.catalyst.harvard.edu…).
Dr. Lo is a physical therapist and research scientist who aims to prevent functional decline and enhance functional independence for older adults with mobility impairments by conducting experimental and translational research. She has expertise and experience in physical therapy, biomechanics, neuroimaging, and neuromodulation.
Dr. Lo has dedicated her career to enhancing functional independence and quality of life in older adults. Her specific research objectives are:
To investigate connections between the brain and body that enable safe navigation throughout daily environments.

Millions of tons of plastic in the ocean aren't floating in plain sight—they're invisible. Scientists have now confirmed that the most abundant form of plastic in the Atlantic is in the form of nanoplastics, smaller than a micrometer. These particles are everywhere: in rain, rivers, and even the air. They may already be infiltrating entire ecosystems, including the human brain, and researchers say prevention—not cleanup—is our only hope.