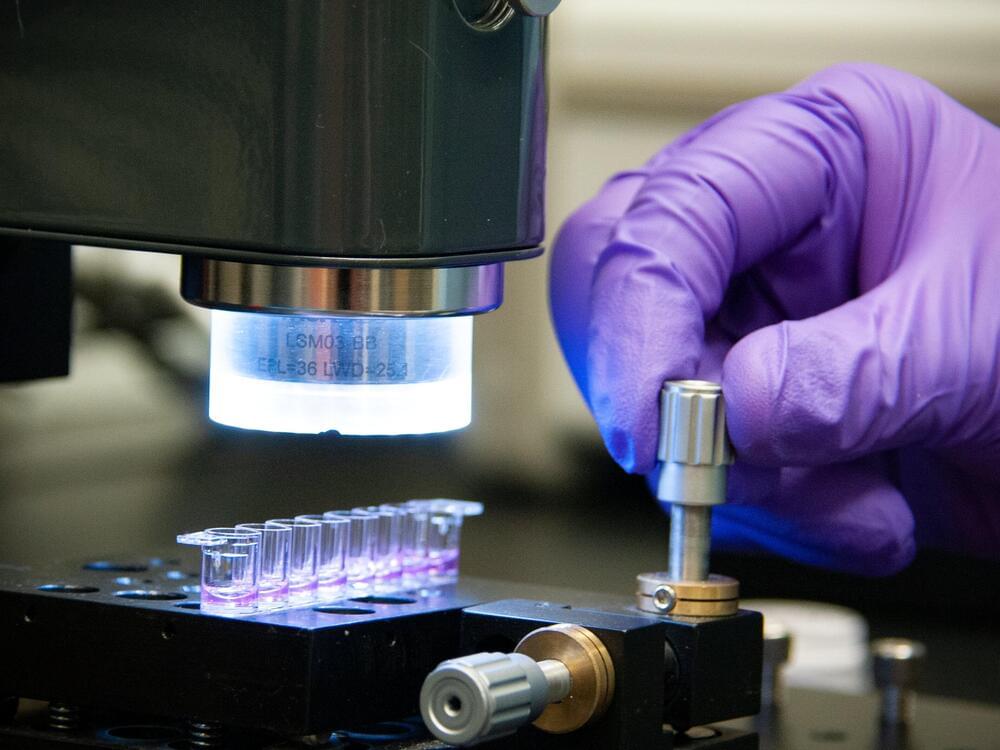
Scientific work often involves sifting through enormous amounts of data, a task that’s overwhelmingly mundane for humans but a piece of cake for artificial intelligence. A new platform dubbed BacterAI can conduct as many as 10,000 experiments per day to teach itself – and us – more about bacteria.
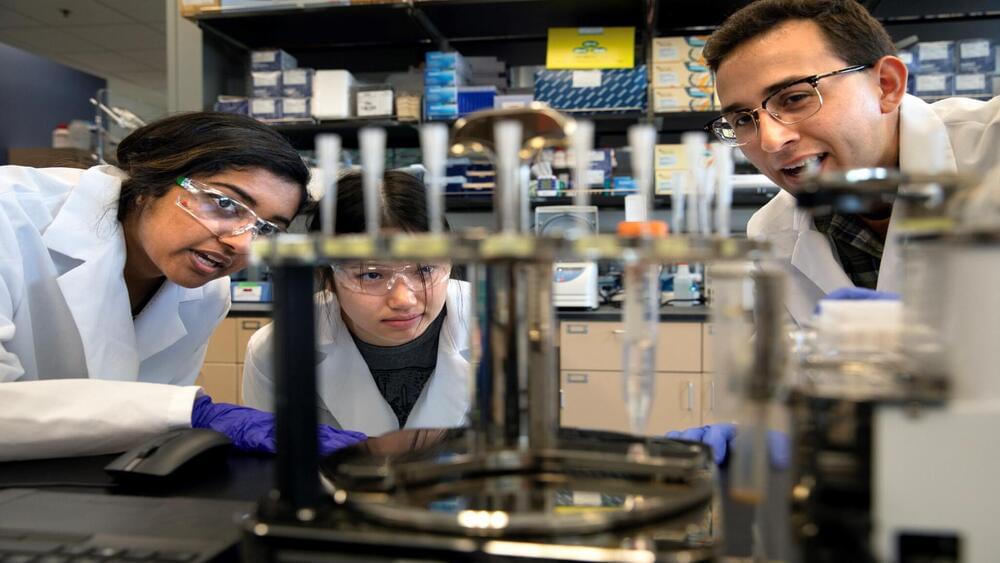
The human body is home to trillions of microbes, covering almost every surface inside and out. Many of them are vital to specific bodily functions, while many others make you sick. Research continues to uncover how inextricably linked our overall health is to our microbiomes, but managing and exploring the data involved remains a daunting task.
“We know almost nothing about most of the bacteria that influence our health,” said Paul Jensen, corresponding author of the new study. “Understanding how bacteria grow is the first step toward reengineering our microbiome.”