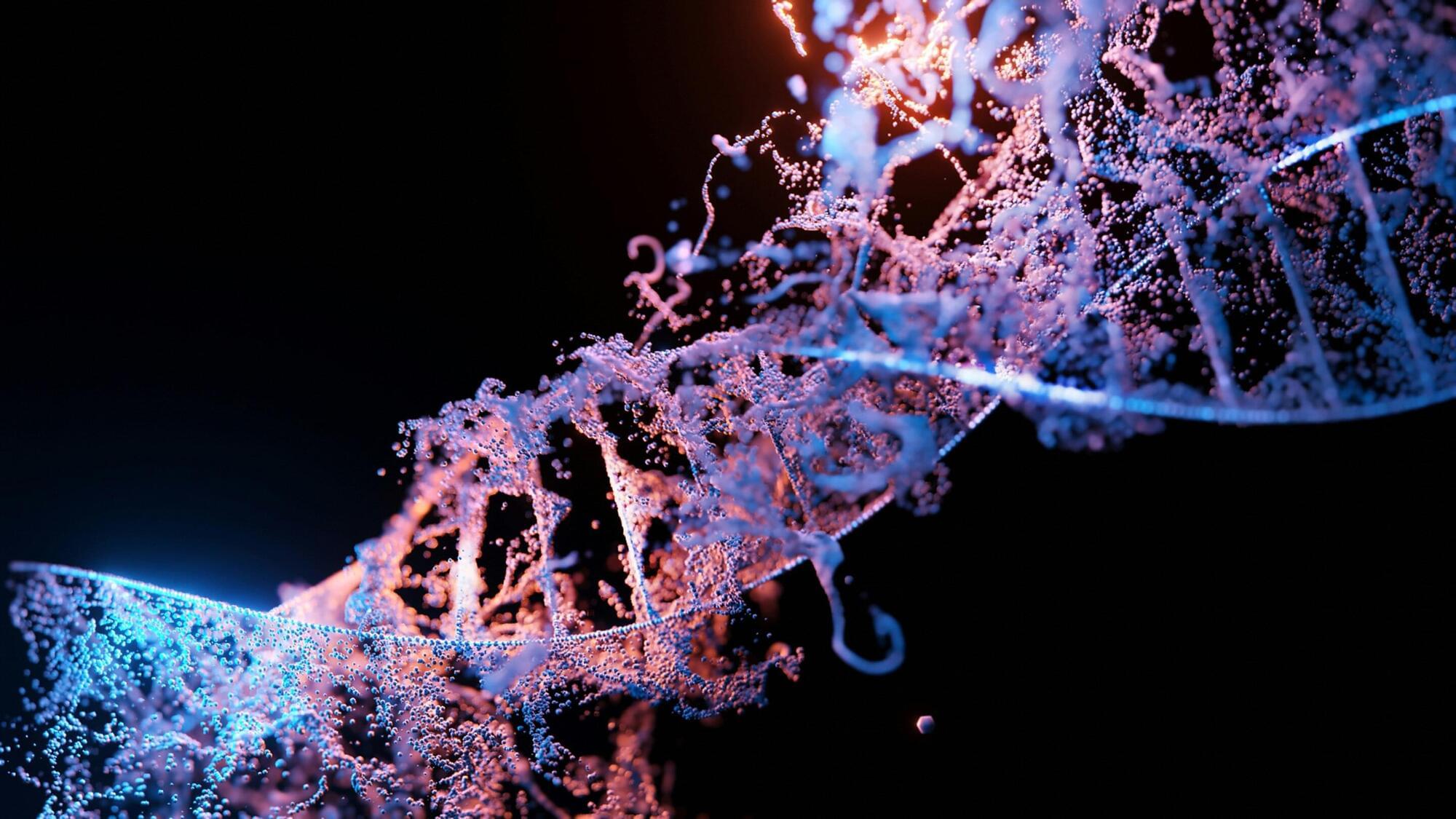
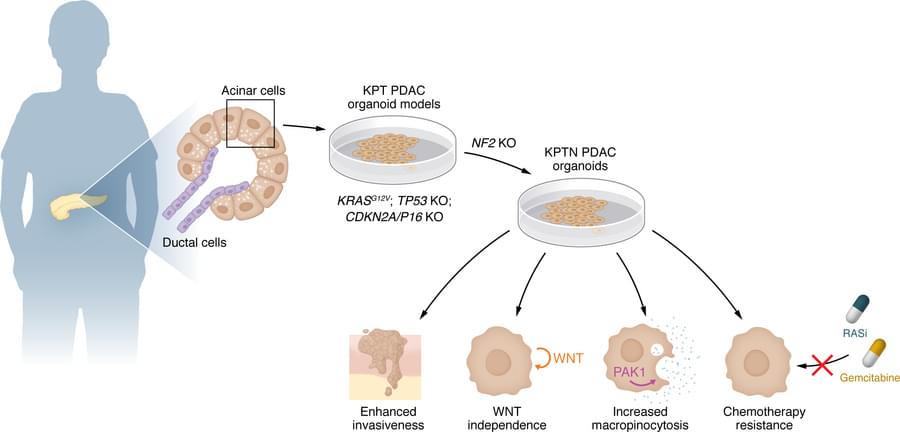
For the first time, researchers at UBC have demonstrated how to reliably produce an important type of human immune cell — known as helper T cells — from stem cells in a controlled laboratory setting. The findings, published today in Cell Stem Cell, overcome a major hurdle that has limited the development, affordability and large-scale manufacturing of cell therapies. The discovery could pave the way for more accessible and effective off-the-shelf treatments for a wide range of conditions like cancer, infectious diseases, autoimmune disorders and more.
“This is a major step forward in our ability to develop scalable and affordable immune cell therapies.”
Dr. Peter Zandstra
Ranked among the world’s top medical schools with the fifth-largest MD enrollment in North America, the UBC Faculty of Medicine is a leader in both the science and the practice of medicine. Across British Columbia, more than 12,000 faculty and staff are training the next generation of doctors and health care professionals, making remarkable discoveries, and helping to create the pathways to better health for our communities at home and around the world.