Kate Broderick discusses the development of INOVIO’s frontrunner COVID-19 DNA vaccine and states the need for preparedness for future outbreaks.



The Space Force’s announcement last week that United Launch Alliance and SpaceX will launch expensive spy satellites and other military payloads brings a long and often fierce battle for government funds to an end — at least for now.
Why it matters: This type of government money — particularly in light of the economic downturn caused by the coronavirus pandemic — is key for space companies that often work on thin margins.
The state of play: ULA was awarded the bulk of the funds — $337 million — for two missions due to launch in 2022, with SpaceX winning $316 million for one mission launching that year.


Tesla’s Model 3 leads the EV sales in China with 11,014 vehicles sold in July. That’s more than the next 3 best-selling EVs combined!
In China this morning, the China Association of Automobile Manufacturers (CAAM) held a press conference in Beijing to update the public on the status of the automotive industry’s recovery.
Overall, it is good news for the market, which managed to recover from the global pandemic much quicker than the rest of the world.
In short, July car production and sales were up from last year – therefore back to growth, but year-to-date is still down roughly 5%:
This video explains DNA packaging, structure of the nucleosome, and histone proteins.

The answer is in their genes—especially those that encode for basic life functions, such as metabolism. Thanks to the lowly C. elegans worm, we’ve uncovered genes and molecular pathways, such as insulin-like growth factor 1 (IGF-1) signaling that extends healthy longevity in yeast, flies, and mice (and maybe us). Too nerdy? Those pathways also inspired massive scientific and popular interest in metformin, hormones, intermittent fasting, and even the ketogenic diet. To restate: worms have inspired the search for our own fountain of youth.
Still, that’s just one success story. How relevant, exactly, are those genes for humans? We’re rather a freak of nature. Our aging process extends for years, during which we experience a slew of age-related disorders. Diabetes. Heart disease. Dementia. Surprisingly, many of these don’t ever occur in worms and other animals. Something is obviously amiss.
In this month’s Nature Metabolism, a global team of scientists argued that it’s high time we turn from worm to human. The key to human longevity, they say, lies in the genes of centenarians. These individuals not only live over 100 years, they also rarely suffer from common age-related diseases. That is, they’re healthy up to their last minute. If evolution was a scientist, then centenarians, and the rest of us, are two experimental groups in action.

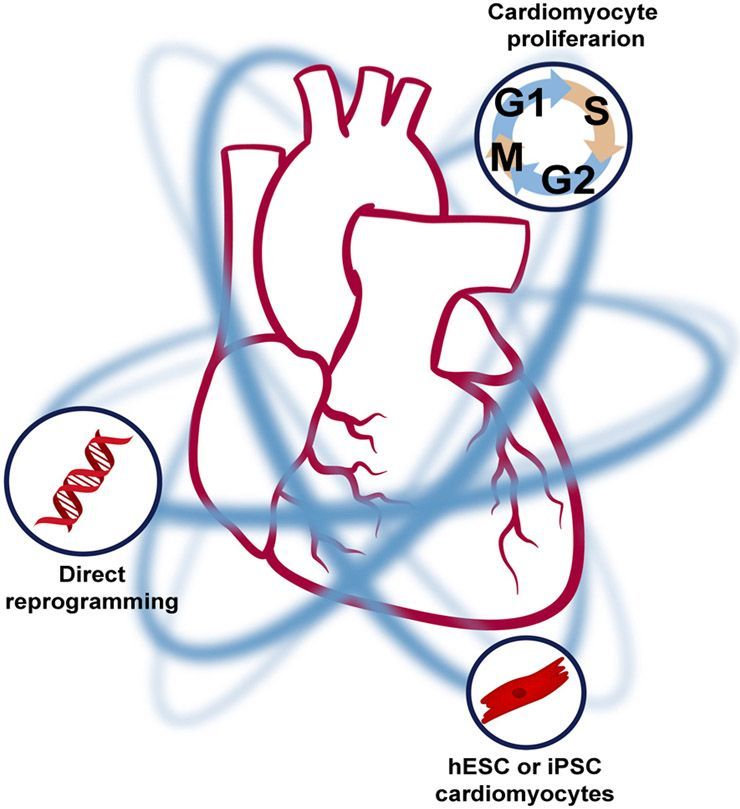
Heart regeneration, a relatively new field of biology, is one of the most active and controversial areas of biomedical research. The potential impact of successful human heart regeneration therapeutics cannot be overstated, given the magnitude and prognosis of heart failure. However, the regenerative process is highly complex, and premature claims of successful heart regeneration have both fueled interest and created controversy. The field as a whole is now in the process of course correction, and a clearer picture is beginning to emerge. Despite the challenges, fundamental principles in developmental biology have provided a framework for hypothesis-driven approaches toward the ultimate goal of adult heart regeneration and repair. In this review, we discuss the current state of the field and outline the potential paths forward toward regenerating the human myocardium.
Cardiovascular diseases have long been the leading cause of death in both industrialized and developing countries. This broad term includes mortality from both vascular and myocardial disease and has been heavily driven by mortality from acute vascular events such as myocardial infarction. This epidemic of vascular death has led to important advances in both basic and clinical research, with significant results. The rates of both myocardial infarction and associated fatalities have been steadily declining (Yeh et al., 2010) thanks to advances in risk-factor management, as well as advanced therapies for coronary revascularization. Unfortunately, myocardial damage from non-lethal cardiac events has contributed to the increased prevalence of cardiomyopathy (Khera et al., 2017; Yeh et al., 2010).
Cardiomyopathy, or weakening of the heart muscle, is a devastating progressive disease with a prognosis worse than that of many malignancies (Mosterd and Hoes, 2007). Decades of advances in understanding the myocardial response to injury have led to the development of safe and effective drugs that slow the progression of cardiomyopathy and even restore function in some reversible cases where there is no significant myocyte loss (Yancy et al., 2017). These drugs mainly target sympathetic activation, afterload, and fibrosis pathways, which are responsible for the progressive nature of the disease after an initial insult. However, to date we have no answer to the disease’s central underlying basis, which is cardiomyocyte loss. The notion that it might be possible to rebuild the cardiac muscle, or to regenerate the myocardium, after injury has sparked significant interest over the past two decades, and it has created a battleground for competing theories and ideas.


Kitasato University Hospital researchers in Japan found that patients with smaller eye pupils were twice as likely to die from heart failure.
Meanwhile, 47 per cent of those with small pupils were readmitted to hospital, compared with just 28 per cent of those with large pupils.
Study author Dr Kohei Nozaki, of Kitasato University Hospital in Japan, said: ‘Our results suggest that pupil area is a novel way to identify heart patients at elevated risk of death or hospital readmission.