There’s only one way to prevent pets from catching this fatal virus.
Category: biotech/medical – Page 2152
Many in-development cures for type 1 diabetes have understandably focused on tackling the autoimmune aspect of the disease before figuring out a way to replace the destroyed beta cells. But what if focusing on the beta cells first could prevent their destruction altogether?
Researchers at Joslin have found that increasing the proliferation and turnover of beta cells before signs of type 1 diabetes could halt the development of the disease. In animal models, researchers in the lab of Rohit N. Kulkarni MD Ph.D., HMS Professor of Medicine and Co-Section Head of Islet and Regenerative Biology in the Joslin Diabetes Center, pushed the growth of beta cells while the animals were still young—meaning organs of the immune system were still developing, and still susceptible to manipulation. The results were published today in Nature Metabolism.
“We are clearly the first to show that if you push the proliferation to continuously generate new insulin producing beta-cells before the immune cell invasion starts then, for some reason we are still trying to figure out, immune cells stop attacking the beta cell,” says Dr. Kulkarni.
A machine learning algorithm can detect signs of anxiety and depression in the speech patterns of young children, potentially providing a fast and easy way of diagnosing conditions that are difficult to spot and often overlooked in young people, according to new research published in the Journal of Biomedical and Health Informatics.
Around one in five children suffer from anxiety and depression, collectively known as “internalizing disorders.” But because children under the age of eight can’t reliably articulate their emotional suffering, adults need to be able to infer their mental state, and recognise potential mental health problems. Waiting lists for appointments with psychologists, insurance issues, and failure to recognise the symptoms by parents all contribute to children missing out on vital treatment.
“We need quick, objective tests to catch kids when they are suffering,” says Ellen McGinnis, a clinical psychologist at the University of Vermont Medical Center’s Vermont Center for Children, Youth and Families and lead author of the study. “The majority of kids under eight are undiagnosed.”
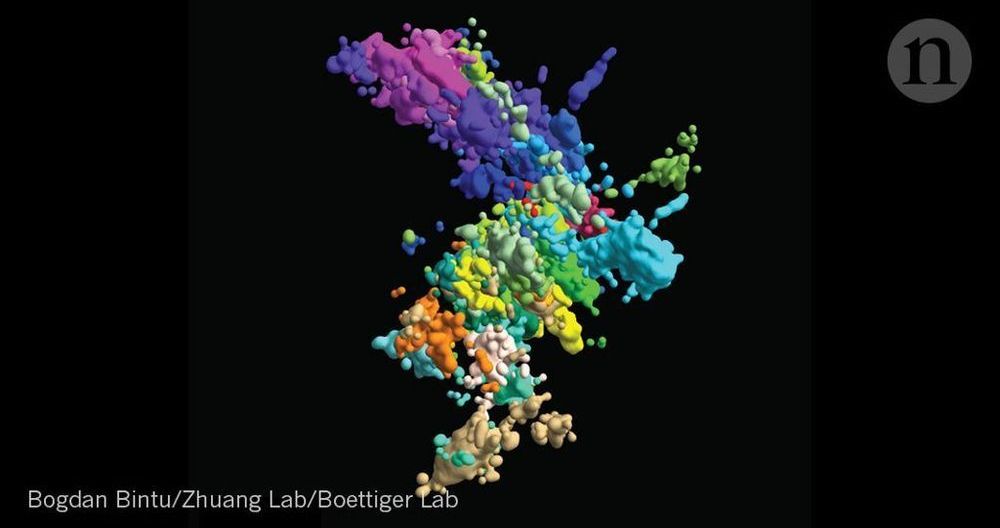
To kill bacteria in the blood, our immune system relies on nanomachines that can open deadly holes in their targets. UCL scientists have now filmed these nanomachines in action, discovering a key bottleneck in the process which helps to protect our own cells.
The research, published in Nature Communications, provides us with a better understanding of how the immune system kills bacteria and why our own cells remain intact. This may guide the development of new therapies that harness the immune system against bacterial infections, and strategies that repurpose the immune system to act against other rogue cells in the body.
In earlier research, the scientists imaged the hallmarks of attack in live bacteria, showing that the immune system response results in ‘bullet holes’ spread across the cell envelopes of bacteria. The holes are incredibly small with a diameter of just 10 nanometres.
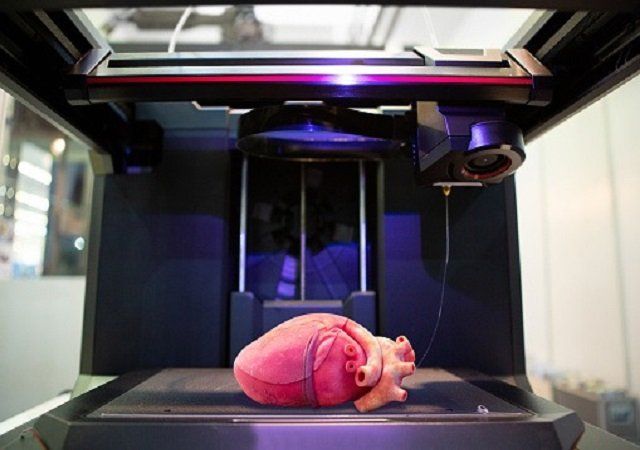
“One of the biggest roadblocks to generating functional tissue replacements has been our inability to print the complex vasculature that can supply nutrients to densely populated tissues,” said Jordan Miller, assistant professor at Rice University in the US.
“Further, our organs actually contain independent vascular networks — like the airways and blood vessels of the lung or the bile ducts and blood vessels in the liver,” Miller said.
“These interpenetrating networks are physically and biochemically entangled, and the architecture itself is intimately related to tissue function. Ours is the first bioprinting technology that addresses the challenge of multi vascularisation in a direct and comprehensive way,” he said.
For most patients, a diagnosis of stage 4 non-small cell lung cancer comes with a dire prognosis. But for patients with specific mutations that cause the disease, there are potentially life-saving therapies.
The problem is that these mutations, known as ALK and EGFR, are not always identified in patients — meaning they never get the treatment.
A new study from the Fred Hutchinson Cancer Research Center in Seattle used machine learning to find these needle-in-a-haystack patients. The idea was to leverage cancer databases to see if patients were being tested for the mutations and receiving these personalized treatments.