Circa 2014
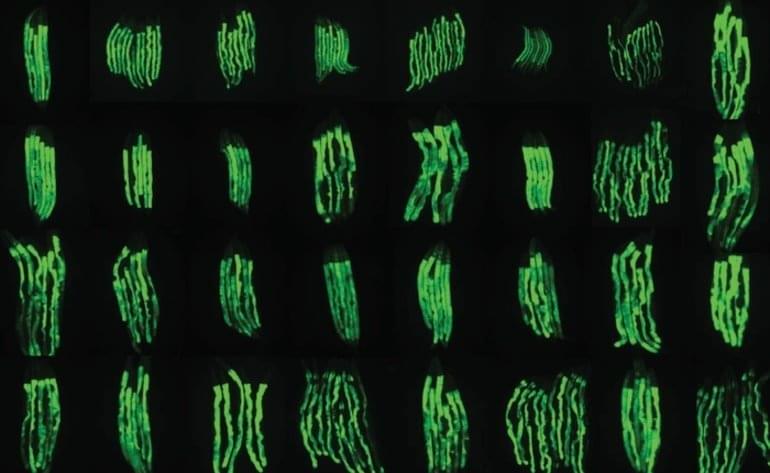
New collaborative research published in the journal Nature Communications by scientists from Japan, Russia and the US contains the genetic analysis on a species of African midge, which can survive a wide array of extreme conditions including large variations in temperature, extreme drought and even airless vacuums such as space. The team successfully deciphered the genetic mechanism that makes the midge invulnerable to these harsh conditions. Prof. Noriyuki Satoh and Dr. Takeshi Kawashima of Prof. Satoh’s Marine Genomics Unit, as well as Prof. Alexander Mikeyhev of the Ecology and Evolution Unit, and Mr. Manabu Fujie and Dr. Ryo Koyanagi of the DNA Sequencing Section at the Okinawa Institute of Science and Technology Graduate University have contributed to the collaboration.
The midge, Polypedilum vanderplanki, is capable of anhydrobiosis, a unique state that allows an organism to survive even after losing 97% of its body water. Anhydrobiotic organisms are also able to survive other severe conditions such as extreme temperatures ranging from 90°C to-270°C, vacuums and high doses of radiation; all of which would be lethal to most other life forms.
The midge found in northern Nigeria lives in an environment where the dry season lasts for at least six months and droughts can last up to eight months. By the time eggs have hatched and larvae have developed, the pools of water they breed in have dried up. However these dried larvae can survive in this dehydrated state for more than 17 years. “This is a very interesting kind of phenomena,” remarks Prof. Satoh. “The first descriptions of this midge were more than 60 years ago… But serious research started only ten years ago.”