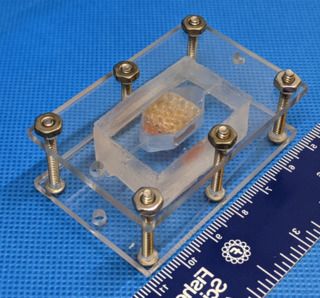
Scientists have successfully grown liver tissue capable of functioning for 30 days in the lab as part of NASA’s Vascular Tissue Challenge.
In 2016, NASA put forth this competition to find teams that could “create thick, vascularized human organ tissue in an in-vitro environment to advance research and benefit medicine on long-duration missions and on Earth,” according to an agency challenge description. Today (June 9), the agency announced not one, but two winners of the challenge.